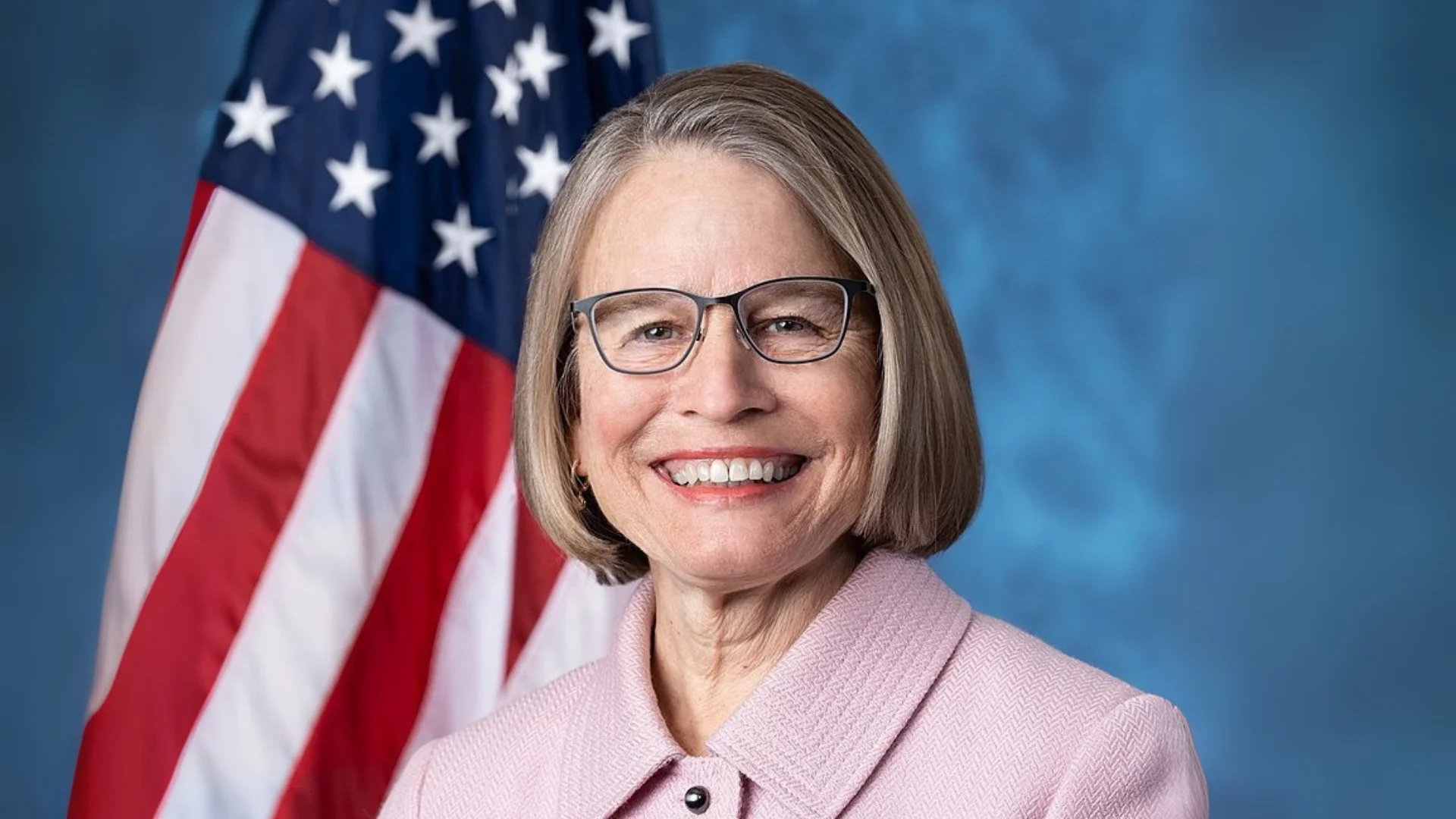
Rep. Mariannette Miller-Meeks Chairwoman at House Committee on Veterans’ Affairs Subcommittee on Health | Wikipedia
Rep. Mariannette Miller-Meeks Chairwoman at House Committee on Veterans’ Affairs Subcommittee on Health | Wikipedia
Rep. Mariannette Miller-Meeks (R-Iowa), Chairwoman of the House Committee on Veterans’ Affairs Subcommittee on Health, opened an oversight hearing today. The session aimed to explore how the Department of Veterans Affairs (VA) and its Community Care program collaborate with private doctors to deliver specialty care to veterans.
"This oversight hearing of the Subcommittee on Health will now come to order," Miller-Meeks began, welcoming members and witnesses. She emphasized the importance of VA's partnership with community providers in meeting veterans' healthcare needs.
Miller-Meeks highlighted that data indicates veterans favor Community Care due to shorter wait times and reduced travel distances for healthcare services. "Polling has shown that Americans want veterans to be able to access shorter wait times and drive times to get their health care," she stated.
The MISSION Act was mentioned as a pivotal measure that addressed gaps in VA's service delivery, particularly in specialty care. This act enabled more resources for veterans through community-based providers, resulting in improved access and efficiency.
Three key indicators were discussed regarding future reliance on community providers for specialty care: increasing demand from women veterans, workforce challenges within VA, and projected changes in demand for various types of care by 2030.
Miller-Meeks noted that by 2040, women are expected to comprise 18% of all veterans, leading to increased demand for both female-specific and general specialty care services. She also pointed out national shortages in healthcare professionals affecting VA facilities.
"V.A. recently identified shortages for clinical roles like psychologists, medical technologists, diagnostic radiologic technologists," she said. This shortage underscores the need for community providers to fill gaps in specialty care provision.
Projections indicate significant shifts in physical space demands across different regions by 2030. For instance, New Orleans may see a decrease while Orlando might experience an increase in needed hospital space.
The hearing also addressed varying regional demands for inpatient acute mental health services. Despite a national decrease projection, some areas could see increases up to 14%.
Miller-Meeks stressed the necessity of timely access to mental health resources and specialty care for veterans: "A condition in need of treatment does not wait for facility infrastructure to catch up."
She concluded by advocating for continued collaboration between VA and community providers: "To best serve veterans, V.A. should pursue whatever gets quality care to veterans when they need it."
The hearing proceeded with remarks from Ranking Member Brownley.





 Alerts Sign-up
Alerts Sign-up